COVID-19 Spike in East Africa: Reflection and 3 things we can learn from Aussie lockdowns.
Uganda, Rwanda, and Kenya are facing a recent surge in new COVID-19 cases and community transmission. Uganda re-imposed COVID-19 restrictions on 7th and 18th June, as it faced a second wave of COVID-19 in response to daily new cases increasing to more than 1000 cases. COVID-19 tests are not free in Uganda, hence the number of daily cases may be an underestimate. Rwanda reimposed restriction on 21st June and recorded 964 new cases on 23rd June, the highest number of new cases in a single day. Kenya reimposed restrictions on 18th June and recorded 622 new cases on 23rd June.
African woman receiving vaccine for COVID-19
Unlike the first wave which significantly affected older people, aged 50 years above, the current wave has been shown to mostly affect younger people aged 20-39. The current COVID-19 strain is reported to have a higher transmission rate and is associated with severe infections. The Director of Health Services in Uganda Dr Henry Mwebesa, noted that it had taken the country less than 10 days to get to a full-blown pandemic with the second wave. This time around, the new confirmed cases are mostly from local transmission including schools, unlike the first wave where most transmission was from returned travellers and cross-country truck drivers.
Vaccination against COVID-19 has been reported to boost immunity against the virus and reduce transmission to others. COVID-19 vaccination rates in East Africa are quite low with less than 2% of the population partly vaccinated in all three countries. This implies that the vast majority of the community are still vulnerable to COVID-19 infection. Therefore, it is crucial for the countries to be diligent in implementing Coronavirus (COVID-19) Standard Operating Procedures (SOPS) including mask-wearing, physical distancing and other precautions against the virus.
Reflection from Melbourne lockdown and 3 lessons that can be applicable to lockdowns in Uganda, Rwanda and Kenya.
Melbourne, Australia’s 112-day lockdown was one of the longest and strictest in the world. The lockdown successfully reduced new confirmed daily cases from more than 725 in August to zero at the end of October in 2020.
First lesson: Collective solidarity; we are in this together; ubuntu – The partnership between the government, public health officials and community members in fighting the pandemic was key. Each person had an important part to play to make the COVID-19 restrictions successful. Therefore, this collective solidarity motivated Melbournians to follow the rules driven by their moral obligation, and social and moral responsibility with everyone doing their bit to protect each other in the community to overcome the pandemic. Following Uganda lockdown 2.0, there have been reports of School COVID-19 clusters where parents were not informed of their children’s symptoms. Similarly, there are stories of workplaces staying silent about infected workers. It is concerning that people ignore their moral responsibility to inform others when they test positive to COVID-19, risking spreading the infection to their close contacts and the wider community. As many have emphasised through social media and MOH public health messages (shown below), the onus is on everyone to disclose their status to close contacts so that they have an opportunity to get tested sooner, self-quarantine and protect their families or work colleagues and the entire community at large.
This is crucial to reduce community transmissions, resultant hospitalisation and ICU admissions and potentially relieve the healthcare system that is already overstretched including healthcare workers who are also significantly affected by the pandemic. The spirit of “ubuntu – I am, because you are” must be emphasised to encourage each of us to protect against and or control the spread of the virus through observing COVID-19 SOPs.
Positive messages of survival, physical support, spiritual support through prayer and coping during and after treatment need to be shared widely to the diverse communities on all media so that the social stigma associated with COVID-19 is stamped out of the community. Our experience dealing with HIV highlighted how stigma stifles prevention and leads to more spread. An environment needs to be created in which COVID-19 and its impact can be discussed and addressed openly, honestly, and effectively.
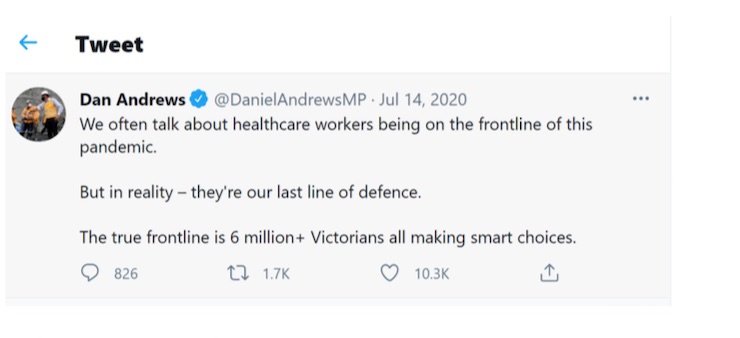
Second lesson: Individuals as first line of defence. Normally, health workers are considered to be the first line of defence in fighting diseases. However, during the Melbourne lockdown 2.0, this analogy was reversed to highlight individuals as the first line of defence and health care workers as the last line of defence. This means the onus is firstly on individuals to do their best and make choices to limit infection and transmission of the virus through limiting contacts, hand-washing, mask wearing, social distancing and getting vaccinated. The impact of individual responsibility in the fight against COVID-19 at the community level is important, reducing the strain on – hospitals overall and relieving health care workers who are the “last line” of defence in the battle against COVID-19.
Third lesson: Daily updates. The community needs to be updated daily on total number of tests taken, the number of new cases, the number hospitalised, the number admitted in ICU, COVID-19 vaccine doses administered each day and cumulative total doses administered. This provides a strong moral platform to motivate people to behave correctly and make individual choices that will drive the numbers downwards at the community level. The authorities need to give clear directions of what is and isn’t allowed, let people know what they want them to do, giving reasons why, when, where and for how long. In Uganda, there has been delayed reporting by the MOH on COVID-19 cases and this creates anxiety and a disconnect in motivation for community members and the health workforce providing care. The latest reporting by the Uganda MOH indicated 859 new cases on 21st June 2021, with a positivity rate of 12%.
Kenya and Rwanda on the other hand provide daily updates on the pandemic (shown above). The daily updates on COVID-19 can be improved by including more information on new hospital admission, new ICU admission and new vaccination doses administered. Providing timely, accurate and reliable updates on COVID-19 is crucial in motivating community participation to fight the pandemic.
By Dr Abimanyi-Ochom Julie and Dr Miriam Marembo | AMA contributors
Dr Julie Abimanyi-Ochom is a lecturer of Public Health at Deakin university in Melbourne (Health Economics, Institute for Health Transformation, Deakin University, Victoria, Australia).
Dr Miriam Marembo is an intelligence officer and data analyst at the Department of Education and Training, Victoria, Australia.